And look what KFF just posted. I think we are ok.

 www.kff.org
www.kff.org
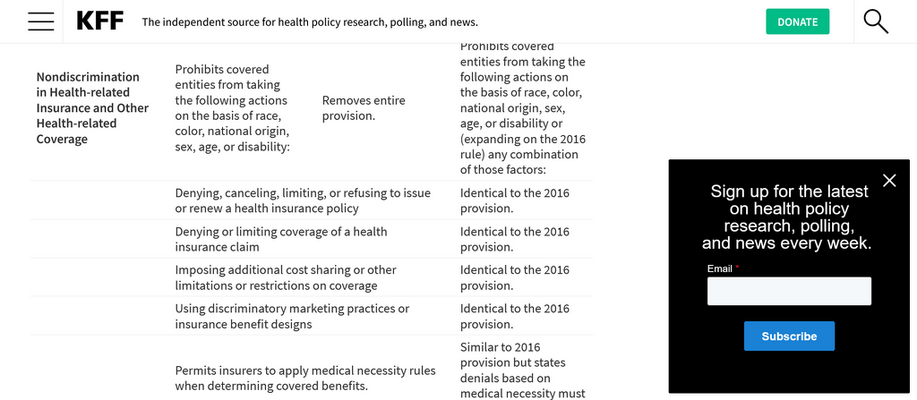

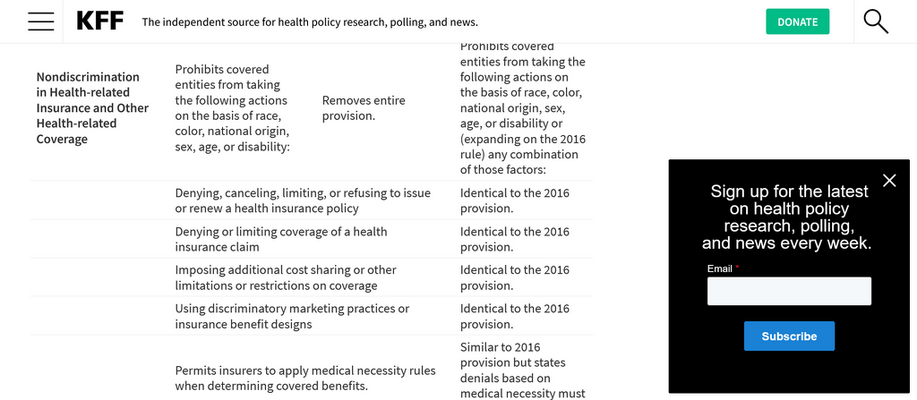
The Biden Administration’s Final Rule on Section 1557 Non-Discrimination Regulations Under the ACA | KFF
This brief overviews the Biden Administration’s 2024 final rule implementing Section 1557 of the ACA, which is home to the law’s major nondiscrimination provisions. It provides a brief background on 1557 rulemaking and identifies key differences between this rule and the 2020 rule from the Trump...